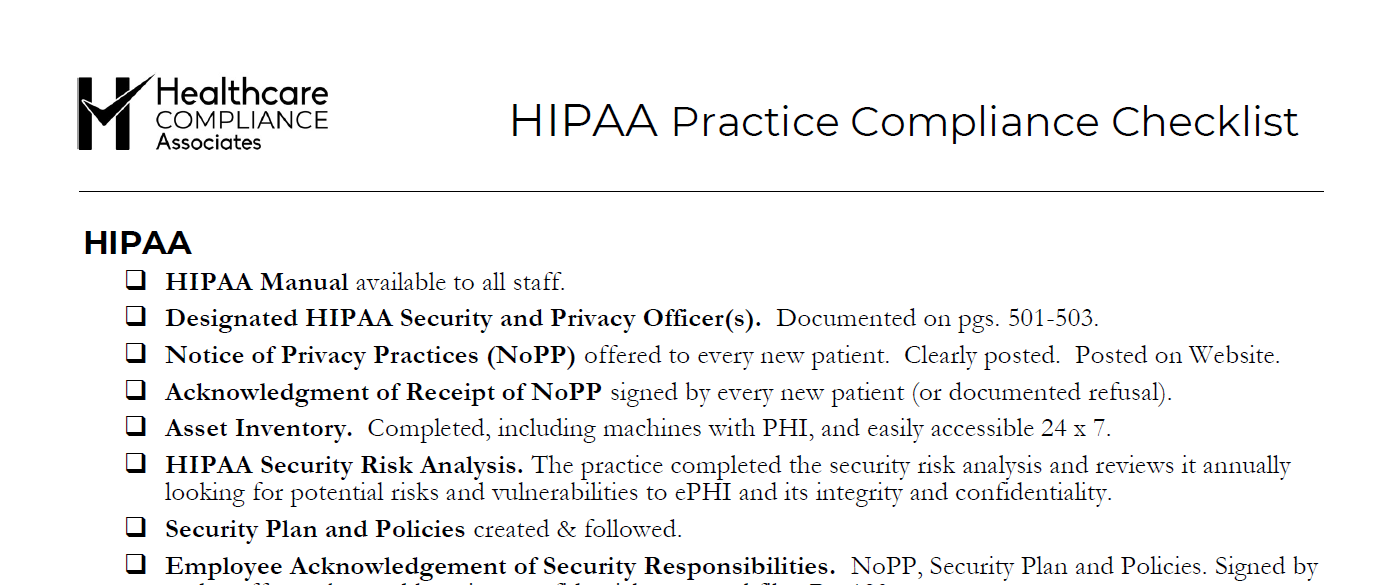
HIPAA Compliance Checklist for Small Healthcare Practices
10-Point HIPAA Checklist
Staying compliant with HIPAA (Health Insurance Portability and Accountability Act) can be daunting for small healthcare practices. With so many rules, regulations, and standards to keep track of, it’s easy to feel overwhelmed. However, ensuring the privacy and security of your patient’s health information is the law and a critical aspect of maintaining trust and professionalism in your practice.
To help simplify the process, we’ve compiled a comprehensive HIPAA compliance checklist for small healthcare practices. This guide will help ensure you cover all the key areas and stay compliant with federal regulations.
1. Conduct Regular Risk Assessments
A HIPAA risk assessment helps you identify potential vulnerabilities in your practice’s handling of patient information. This includes assessing how you collect, store, and transmit Protected Health Information (PHI). Make sure your risk assessments are thorough and conducted at least annually, or whenever there are major changes to your systems.
Key Points:
- Identify risks to PHI confidentiality, integrity, and availability.
- Document all findings and develop a plan to mitigate risks.
- Reassess risks regularly to stay ahead of potential threats.
2. Ensure Employee Training
HIPAA compliance is a team effort; all employees must understand the regulations. Regular training ensures that everyone in your practice, from front-office staff to healthcare providers, knows how to handle PHI properly and what to do in case of a data breach.
Key Points:
- Conduct annual HIPAA training for all employees.
- Provide role-specific training based on job duties.
- Keep records of completed training sessions.
3. Implement Safeguards for Electronic PHI (ePHI)
The Security Rule of HIPAA requires healthcare providers to implement safeguards to protect ePHI. This involves both physical and technical measures to prevent unauthorized access to digital health information.
Key Points:
- Use encryption to protect ePHI during transmission.
- Implement secure access controls, such as strong passwords and multi-factor authentication.
- Regularly update and patch software to address security vulnerabilities.
4. Create and Maintain HIPAA Policies and Procedures
Every small healthcare practice must have written policies and procedures that outline how PHI is handled. These documents should cover everything from patient consent forms to how data breaches are reported and handled.
Key Points:
- Ensure that policies are up-to-date and reflect current regulations.
- Make these policies available to all employees.
- Review and update your policies regularly.
5. Have a Breach Notification Plan
If a data breach occurs, HIPAA requires that you notify the affected patients and report the breach to the Department of Health and Human Services (HHS). Having a well-documented breach notification plan ensures that you can respond quickly and correctly.
Key Points:
- Develop a breach response plan that includes internal reporting and external notifications.
- Know the timeline for breach reporting (within 60 days of discovery).
- Keep patients informed of any actions you are taking to remedy the situation.
6. Secure Physical Access to PHI
While much of HIPAA compliance focuses on digital data, physical security is just as important. Ensure that any paper records, filing systems, and workstations with access to PHI are secure.
Key Points:
- Lock offices, filing cabinets, and storage rooms that contain PHI.
- Limit access to areas where PHI is stored to authorized personnel only.
- Implement clean desk policies to ensure no PHI is left unattended.
7. Maintain a Business Associate Agreement (BAA)
Small healthcare practices often work with third-party vendors, such as billing services or IT providers. If any of these vendors have access to PHI, you must have a signed Business Associate Agreement (BAA) in place. This document outlines the vendor’s responsibility to protect PHI and ensures they comply with HIPAA regulations.
Key Points:
- Ensure BAAs are signed by all relevant vendors.
- Review and update BAAs regularly to maintain compliance.
- Keep records of all signed agreements.
8. Appoint a Privacy and Security Officer
Even small healthcare practices must designate someone responsible for overseeing HIPAA compliance. This could be a specific employee or an outsourced professional. The Privacy Officer handles compliance with the HIPAA Privacy Rule, while the Security Officer oversees compliance with the Security Rule.
Key Points:
- Clearly define the roles and responsibilities of the Privacy and Security Officer.
- Ensure they have the necessary training and resources to manage compliance.
- Regularly review your practice’s compliance efforts with the appointed officer.
9. Monitor Access to PHI
One of the most important aspects of HIPAA compliance is ensuring that only authorized individuals have access to PHI. Implementing audit controls and monitoring systems can help you track access to both physical and digital records.
Key Points:
- Implement audit trails to track who accessed or modified PHI.
- Review access logs regularly for any suspicious activity.
- Address unauthorized access immediately to prevent data breaches.
10. Regularly Review and Update Compliance Practices
HIPAA regulations can change, and new threats to patient data emerge over time. Regularly reviewing and updating your compliance practices is essential to staying compliant and protecting your patients’ information.
Key Points:
- Schedule periodic reviews of your HIPAA policies and procedures.
- Stay informed of any changes to HIPAA regulations.
- Make updates as necessary to ensure your practice stays compliant.
Final Thoughts
HIPAA compliance doesn’t have to be overwhelming for small healthcare practices. By following this comprehensive checklist, you can create a solid foundation for protecting your patients’ health information and staying compliant with federal regulations. Regular assessments, employee training, and safeguarding both physical and electronic PHI are key to ensuring your practice remains HIPAA compliant.
If you need assistance with HIPAA compliance or want to ensure your practice is fully protected, contact Healthcare Compliance Associates today. We specialize in making compliance simple, efficient, and stress-free for healthcare practices of all sizes.